What is Asystole?
The term asystole simply refers to an absence of ventricular activity, which means the patient will exhibit no discernible electrical activity on an ECG readout. In most cases, asystole is a lethal arrhythmia and survival is extremely rare.
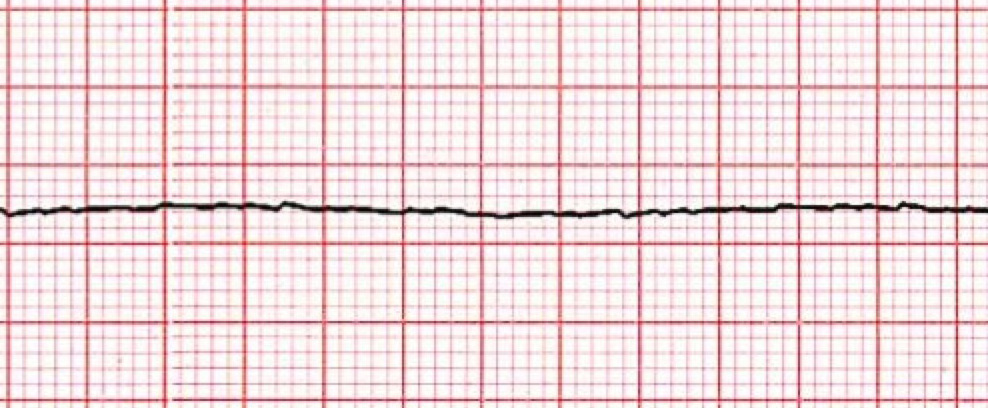
Asystole is a cardiac standstill. It is represented by a straight flat, or almost flat, line on an ECG. However, ACLS providers should not rely on an ECG readout alone for their diagnosis of a patient in cardiac arrest. It’s always a good idea to confirm it clinically because what appears to be a flat line on the ECG, can also be caused by a loose ECG lead.
ACLS providers should confirm that the flat line on the monitor is indeed true asystole by validating that the flat line is:
- Not another rhythm, such as fine VFib masquerading as a flat line
- Not the result of an operator error
Asystole ECG Readout
-
The Heart Rhythm
The first thing ACLS providers should do is look at the patient’s heart rhythm. Does the heart rhythm look regular? Or does it look irregular? In the ECG above, there is no heart rhythm.
-
The Heart Rate
Next, they’ll want to look at the heart rate of the patient. What is the patient’s heart rate? Is it normal? Or is it too slow or too fast? In this case, the patient has no rate and no pulse.
-
P-Wave
After looking at the heart rate, healthcare providers should check to see if the patient’s P-waves look normal by asking themselves the following questions.
• Are the patient’s P-waves present? No, making any other questions about QRS non-applicable. However, in some cases, a small P-wave can be seen but it isn’t followed by any other waveforms.
Healthcare providers may notice small P-waves on the ECG that aren’t followed by any other waveforms. When present, this can mean that (in rare cases) the atrial pacemaker may be trying to send an impulse but has no ventricular reaction.
-
PR Interval
Next, ACLS providers should look at the PR interval on the patient’s ECG readout and ask themselves the following questions:
• Is the PR interval normal, meaning between .12 and .20 seconds or is it contained within one large square on the readout? The answer is no because there isn’t a PR interval.
• Is the PR interval constant? Again, this is non-applicable since there isn’t a P-wave. -
QRS Complex
The last thing ACLS providers should look at to determine if the sinus rhythm is normal or not is the QRS complex, asking themselves these questions while they do:
• Is the QRS interval less than .12 seconds? No. There is no evidence of a QRS complex, making any other questions about QRS non-applicable.
Clinical Significance
What is the cardiac interpretation based on the ECG readout above? Based on these questions and the findings from the ECG readout, it would appear that this patient is in asystole. Because there is no myocardial, electrical, or mechanical activity, there is no pulse and no circulation of blood and oxygen.
Asystole is most commonly seen following a period of unconverted ventricular fibrillations or ventricular tachycardia. And while asystole is most commonly seen after extended, untreated, and sudden cardiac arrest, it can also be caused by reversible conditions, known as the H’s and T’s:
Common Causes of Asystole – the H’s
- Hypovolemia
- Hypoxia
- Hydrogen ion or acidosis
- Hypokalemia
- Hyperkalemia
- Hypothermia
Common Causes of Asystole – the T’s
- Tension pneumothorax
- Tamponade (cardiac)
- Toxins
- Thrombosis (pulmonary)
- Thrombosis (coronary)
Asystole Algorithm
The cardiac arrest algorithm consists of two pathways. The left side of the algorithm outlines treatment for a shockable rhythm, like VFib or pulseless V-tach, while the right side of the algorithm outlines treatment for non-shockable rhythms, like asystole or pulseless electrical activity (PEA).
In both pathways, all of the treatments are designed around two-minute periods of uninterrupted, high-quality CPR.