What is Asystole?
Asystole, sometimes referred to as a flat line on the monitor, represents an absence of both electrical and mechanical activity in the heart. It’s important to understand that if a patient has no pulse and this is confirmed in one lead, there are a few things ACLS providers can double-check to confirm this, such as asking the following questions:
- Are all the leads on correctly?
- Are all the leads attached to the patient with good contact?
- Does the ECG have a sufficient power supply?
- Is the amplitude set correctly to determine asystole vs. fine VFib?
Like pulseless electrical activity (PEA), it’s also important to determine what may have caused the patient’s asystole, or in other words, examine the H’s and T’s. If you can figure out why the patient went into cardiac arrest, looking at the H’s and T’s will help you determine the possibility of treating any reversible causes of the asystole.
The H’s and T’s are:
- Hypovolemia
- Hypoxia
- Hydrogen ion (acidosis)
- Hypokalemia
- Hyperkalemia
- Tension pneumothorax
- Cardiac tamponade
- Toxins
- Cardiac thrombosis
- Coronary thrombosis
Treatment of asystole is not limited to the interventions outlined in the asystole algorithm. ACLS providers must attempt to identify and correct an underlying cause if one is present.
Healthcare providers must stop and ask themselves, Why did this patient have this cardiac arrest at this time. It’s essential to search for and treat reversible causes of asystole in order for a healthcare provider’s resuscitative efforts to be successful.
That is the role of the H’s and T’s in a nutshell: to identify conditions that could have contributed to their asystole.
Asystole ECG Readout
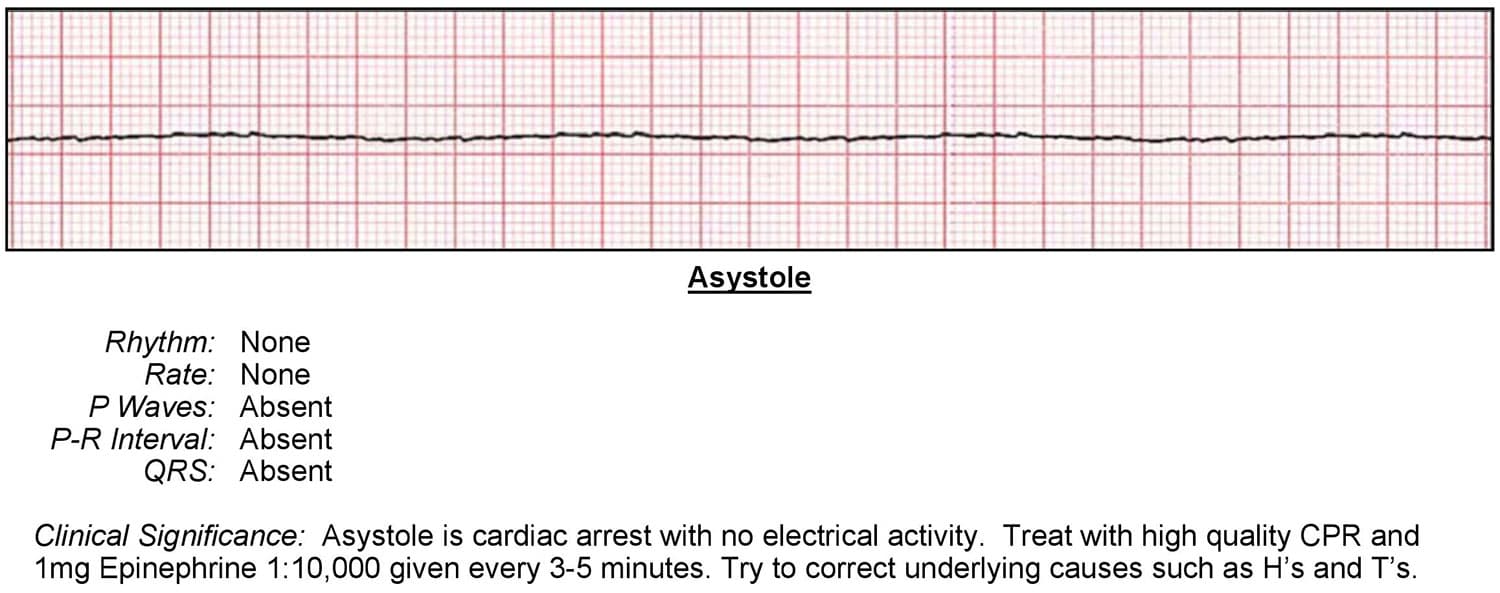
Heart rhythm: None
Heart rate: None
P-waves: Absent
P-R interval: Absent
QRS: Absent
Clinical Significance
Based on the findings from the ECG readout above, it would appear that this patient is in asystole. Because there is no myocardial, electrical, or mechanical activity, there is no pulse and no circulation of blood and oxygen.
Asystole Treatment
The treatment of asystole consists of the following components:
- Implementing the steps in the cardiac arrest algorithm
- Identifying and correcting underlying causes – the H’s and T’s
- Terminating resuscitation efforts if appropriate
Asystole is not a shockable rhythm. So, treatment will involve high-quality CPR, airway management, IV or IO therapy, and medication therapy – specifically 1mg of epinephrine 1:10,000 concentration every 3 to 5 minutes via rapid IV or IO push.
Asystole Treatment Steps
- ACLS providers perform their initial assessment, which involves the following:
• Perform high-quality CPR
• Establish an airway and provide oxygen to keep oxygen saturation levels above 94 percent
• Monitor the patient’s heart rhythm and blood pressure - Continue high-quality CPR for two minutes, while also attempting to establish IV or IO access.
- Give 1mg of epinephrine as soon as possible and every 3 to 5 minutes.
- After two minutes of CPR, check the patient’s rhythm.
- If the monitor and assessment show V-tach or VFib, move to the appropriate algorithm for each.
- Evaluate and treat reversible causes (the H’s and T’s).
- If the patient attains ROSC (return of spontaneous circulation), provide Post Cardiac Arrest Care
It is rare for asystole to be reversed, especially after a long duration. If the patient does not respond to the BLS and ACLS treatments, the rescue team will need to decide when to stop resuscitative efforts. If there is a high degree of certainty that the patient will not respond to further ACLS interventions, it would be appropriate to stop.
Asystole often represents the patient’s final rhythm. Their cardiac function has diminished to a point when all electrical and functional cardiac activity finally stops and the patient dies. (Asystole is also the final rhythm of a patient initially in VFib or pulseless V-tach.) Prolonged efforts are unnecessary and futile unless special resuscitation situations exist, such as hypothermia and drug overdose.
The decision to stop resuscitative efforts must be based on specific protocols and the consideration of time from collapse to CPR, time from collapse to first defibrillation attempt, underlying causes, response to resuscitative measures, and an ETCO2 less than 10 after 20 minutes of CPR.