What is the Bradycardia Algorithm?
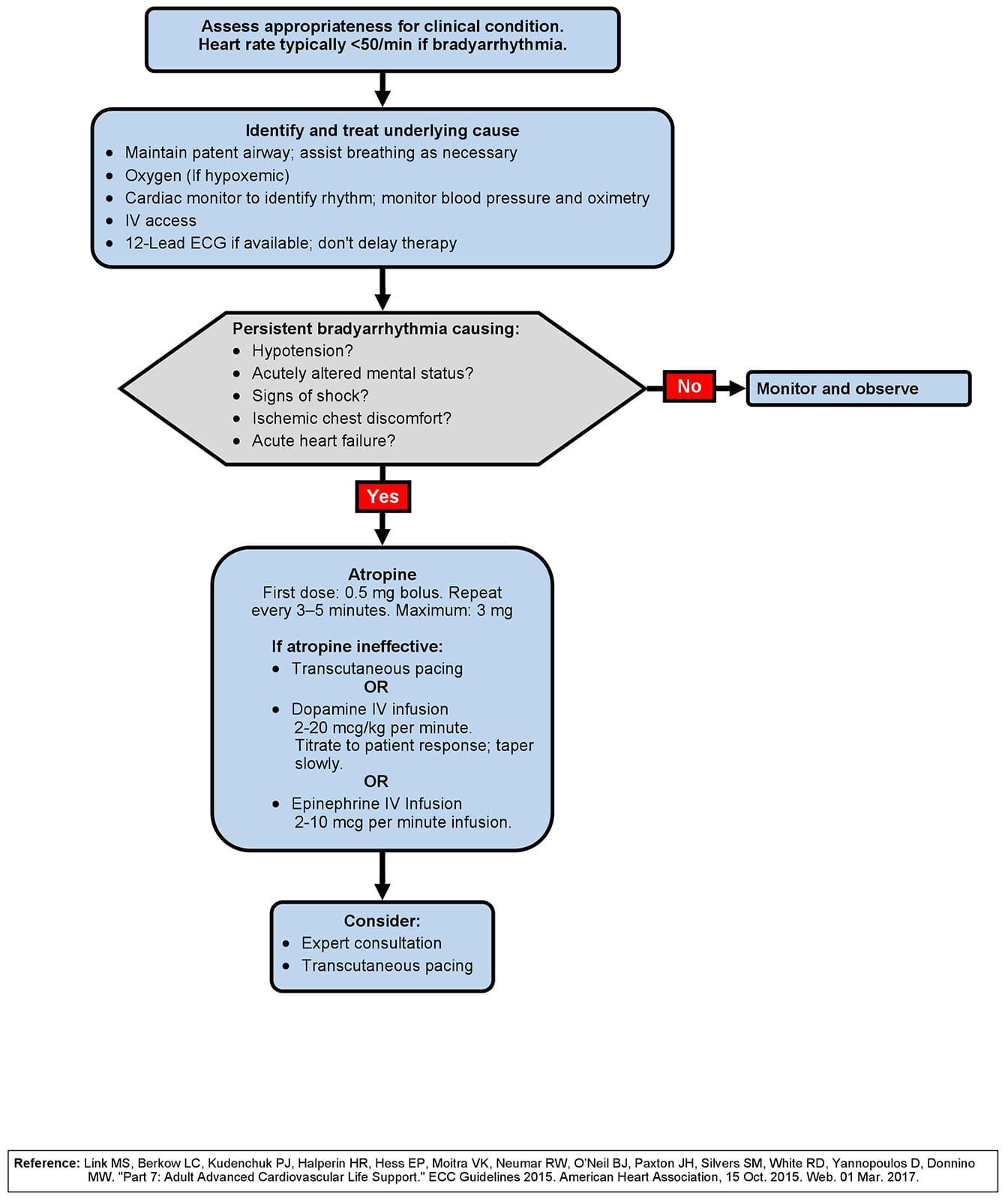
The adult bradycardia algorithm outlines the steps for the assessment and management of a patient presenting with symptomatic bradycardia with a pulse. The implementation of the bradycardia algorithm begins with the identification of bradycardia.
The first steps after identifying the bradycardia include the components of the BLS assessment and the primary assessment, such as supporting circulation and airway management, giving oxygen if indicated, monitoring the rhythm and vital signs of the patient, establishing IV access, and obtaining a 12-lead ECG if available.
The key clinical question is whether the bradycardia is causing the patient’s symptoms or some other illness is causing the bradycardia.
What is Bradycardia?
Absolute bradycardia is defined as a pulse rate less than 60 beats per minute. During the initial patient assessment, ACLS providers must determine whether any life-threatening signs and symptoms are present that have been caused by that bradycardia.
Bradycardia can present itself in several different cardiac rhythms, which include sinus bradycardia and varying degrees of AV heart blocks.
To identify whether a patient has bradycardia, ACLS providers should first check to see that bradycardia is present, as in a heart rate less than 50 beats per minute, and also ask themselves if the patient’s bradycardia is inadequate for the patient’s condition – functional vs. relative bradycardia.
Bradycardia Signs and Symptoms
Step three of the bradycardia algorithm prompts healthcare providers to consider if the patient’s signs or symptoms of poor perfusion are caused by the bradycardia. Key clinical questions that ACLS providers should ask themselves are:
- Does this patient have serious signs or symptoms?
- Are the signs and symptoms related to the patient’s slow heart rate?
ACLS providers should also look for adverse signs and symptoms of the bradycardia which include:
- Chest discomfort
- Shortness of breath
- Decreased level of consciousness
- Weakness
- Fatigue
- Light-headedness or dizziness
- Hypotension
- Congestive heart failure
- Ventricular arrhythmias related to the bradycardia
- Acutely altered mental status
- Signs of shock
Sometimes the symptom is not due to the bradycardia. For example, hypotension associated with bradycardia may be due to myocardial dysfunction rather than the bradycardia. Healthcare providers should keep this in mind when they reassess the patient’s response to treatment.
Regardless of the patient’s rhythm, if their heart rate is too slow and the patient has symptoms from that slow heart rate, the bradycardia should be treated to increase the heart rate and improve perfusion, following the steps of the bradycardia algorithm below.
The primary decision point in the bradycardia algorithm is the determination of adequate perfusion. If the patient has adequate perfusion, ACLS providers should observe and monitor the patient.
If the patient has poor perfusion, atropine would be the first drug of choice. If atropine is ineffective, healthcare providers should prepare for transcutaneous pacing (TCP) or consider a dopamine or epinephrine infusion.
Bradycardia Algorithm & Treatment
For asymptomatic patients, ACLS providers should continue to provide care with close monitoring and choose which appropriate treatment and care should be given.
The primary treatment for symptomatic bradycardia includes the following:
- Administration of supplemental oxygen if the patient’s pulse oximetry is below 94 percent and establishes IV access.
- Monitor the patient’s ECG rhythm.
- Obtain a 12 lead as soon as possible, but don’t delay therapy to get it.
- Administration of atropine at .5mg via rapid IV push to increase the patient’s heart rate.
- If atropine is proving to be ineffective, consider transcutaneous pacing.
If there are serious signs and symptoms that the patient is unresponsive, the first line of treatment should be transcutaneous pacing rather than atropine. - Consider the administration of other medications such as:
a. An epinephrine infusion at between 2 to 10mcg per minute
b. A dopamine infusion at between 5 and 10mcg per kg per minute
When ACLS providers are dealing with a conscious patient who needs transcutaneous pacing, they should consider sedation first to help alleviate the patient’s discomfort.
Some patients may present with relative bradycardia when their heart rate is over 60 beats per minute, but they present with low blood pressure or decreased level of consciousness. In these cases, the same interventions would be required as a patient with absolute bradycardia.
Adult Bradycardia With a Pulse Algorithm